Atrial fibrillation (AFib or AF) is a big hairy heart deal. For decades, doctors believed it affected more than 3 million American Adults. Then the CDC suggested that as many as six million Americans suffered from this irregular heart rhythm. A new study of 30 million people receiving healthcare in California indicates that almost 5% of the US population actually has AFib. That amounts to 10.5 million US adults. The study was published in the Journal of the American College of Cardiology, Sept. 11, 2024. Yikes! What is going on?
Atrial Fibrillation Is Going Up Fast!
A decade ago cardiologists were estimating that cases of atrial fibrillation would double to 12 million people by 2030 (American Journal of Cardiology, Oct. 15, 2013). We are almost there and we are still well-short of 2030.
The authors of the new research point out that (Journal of the American College of Cardiology, Sept. 11, 2024):
“The number of patients with a diagnosis of AF in California has markedly increased over time.
“Even earlier reports of AF described before the contemporary period suggested that AF rates were rising, and investigations outside of the United States have reported similar trends. This has been attributed to a combination of factors, including population growth and aging, increasing prevalence of risk factors for AF in many populations, improved survival, and enhanced AF detection.”
Conclusions:
“The prevalence of AF has risen substantially in recent years, exceeding prior predictions pertinent to the current era. We estimate that there were ∼10.55 million adults with diagnosed AF in the United States in 2019. Given the adverse consequences and considerable health care utilization associated with the disease, this rising prevalence calls for greater resource allocation and more efficient prevention and treatment strategies to curb the increasing burden of AF in the United States.”
A older review in the Mayo Clinic Proceedings (December, 2016) also concludes:
“Atrial fibrillation (AF) is the most common sustained arrhythmia in adults, and its prevalence is expected to increase 3-fold in the next 3 decades. Experts now characterize these epidemiological trends as an AF epidemic.”
What’s Causing the AF Epidemic?
The most common answer is age. Older people are more susceptible to atrial fibrillation than younger people. Populations are aging. But that doesn’t really tell us what’s behind this fast growing epidemic.
Some hypothesize that it’s due to increases in blood pressure. But the data suggest that rates of hypertension have stabilized due in large part to improved blood pressure control (JAMA, May 26, 2010). Therefore one might argue that blood pressure is probably not responsible for the dramatic increase in AF incidence.
Some experts suggest that obesity and diabetes could be contributing risk factors (European Heart Journal. Cardiovascular Pharmacotherapy, Apr. 2016). It is not clear, though, that weight reduction and tight glucose control could reverse the AF epidemic. Other risk factors that have been proposed include heart failure, hyperthyroidism and kidney disease.
AFib Anomalies:
Experts cannot explain the following:
- White people are more likely to develop atrial fibrillation than African Americans and Latinos. That’s despite the fact that African Americans and Latinos are more likely to suffer from overweight, diabetes and hypertension.
- There is twice as much AFib in developed regions compared to developing countries (Circulation, Feb. 24, 2014). Australia, Western Europe, Scandinavia and the United States have much higher rates of this arrhythmia than countries like Brazil, China, Colombia, India, Mexico, Peru or Russia.
Why We Should Care About AFib!
Atrial fibrillation has become a huge public health problem. That’s because this arrhythmia greatly increases the risk of hospitalization, stroke and death. The annual medical cost of AFib in the U.S. could be as high as $26 billion! It is estimated that each American with AFib could run up a tab of $8,705 a year (Circulation. Cardiovascular Quality and Outcomes, May, 2011). That is a budget buster for individuals, insurance companies and tax payers (think skyrocketing Medicare costs).
This does not take into account human suffering. People with AFib can suffer life-threatening complications because of this irregular heart rhythm. More about that below. And the treatments are not benign. Drugs to control this arrhythmia have some pretty serious side effects. You can learn more about the hazards of amiodarone at this link. And anticoagulants like apixaban (Eliquis), dabigatran (Pradaxa), rivaroxaban (Xarelto) and warfarin (Coumadin) carry their own risks. More about that at this link.
What is Atrial Fibrillation?
AFib happens when the upper chambers of the heart don’t function properly. Blood can pool, allowing clots to form. These blood clots can then be pumped to the brain and cause severe damage.
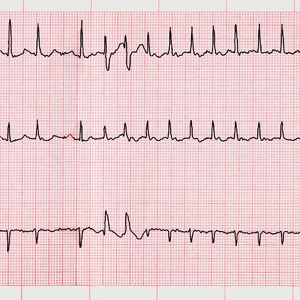
Symptoms of AFib include shortness of breath, fatigue, lightheadedness, chest pain and palpitations (a feeling of pounding or fluttering in the chest). An electrocardiogram is used to diagnose this arrhythmia. An app, Kardia from AliveCor, can be installed on a smart phone to detect this irregular heart rhythm.
Drug-Induced AF: The Elephant in the Room
One risk factor that is often overlooked when AFib is discussed in the medical literature is medication. A surprising number of drugs may increase the chance of developing atrial fibrillation.
Cortisone-type Drugs:
Millions of people take high doses of corticosteroids such as prednisone for a variety of health conditions including asthma, sinusitis, COPD, severe skin reactions and rheumatoid arthritis. A study in JAMA Internal Medicine (May 8, 2006) concluded that people taking cortisone-type drugs were significantly more likely to develop AFib. The researchers encourage physicians to monitor people for abnormal heart rhythms while receiving corticosteroids.
NSAIDs and AFIB:
Other drugs that can also trigger this AFib include the nonsteroidal anti-inflammatory drugs (NSAIDs) that so many people take to relieve pain. Drugs like diclofenac, ibuprofen and naproxen increase the risk of developing AFib by up to 80 percent (BMJ Open, Apr. 8, 2014). According to the senior author of this Dutch study, Dr. Bruno H. Stricker:
“I would really strongly advise that older people be very careful with using these drugs. They don’t do anything except relieve pain. Pain is a nuisance, but dying is a nuisance, too.”
Mineral Depletion and AFib:
People who take NSAID-type pain relievers are at greater risk for heartburn and stomach ulcers. They may turn to acid-suppressing drugs such as esomeprazole (Nexium), lansoprazole (Prevacid) and omeprazole (Prilosec) for relief. Such proton pump inhibitors can deplete the body of magnesium if they are taken for long periods of time. When magnesium levels drop, atrial fibrillation is a potentially serious complication.
Diuretics used to lower blood pressure may also lower magnesium and potassium levels. This could also put some people at risk for atrial fibrillation. This is a classic catch-22. If hypertension increases the risk of AF, the appropriate treatment would be blood pressure lowering drugs. But the most commonly prescribed drugs, diuretics, might actually increase the risk of AF due to depletion of key electrolytes.
Other Drugs and AFib:
According to the Journal of the American College of Cardiology (Dec. 2004), other drugs that have been linked to AFib include antidepressants (fluoxetine, tranylcypromine and trazodone), an antipsychotic (clozapine), migraine medicine, (sumatriptan) and medication for erectile dysfunction (sildenafil). Certain cancer drugs and some medications used to treat heart problems may also precipitate AFib (Kaakeh et al, Drugs, Aug. 20, 2012).
Drugs that make the heart beat faster can make a person more susceptible to AFib, but so can drugs that slow the heart rate. Turkish doctors reported on a person whose AFib was triggered by the combination of beta-blockers and diltiazem (Altunbas et al, Journal of Atrial Fibrillation, Oct. 31, 2016).
The Take Home Message:
When cardiologists are consulted because a patient has atrial fibrillation, they frequently prescribe anticoagulants or antiarrhythmics. They may also recommend an ablation procedure to try to correct the underlying arrhythmia. These are valuable treatments, but there are risks associated with surgery as well as drug treatment.
People on anticoagulants walk a tightrope. On one side is the risk of a blood clot that could cause a thrombotic stroke. On the other side is excess bleeding that could cause a hemorrhagic stroke. This is a very careful balancing act.
Perhaps doctors should start any evaluation of atrial fibrillation by carefully reviewing the patient’s list of medications. Drugs that can predispose a person to AFib should be reviewed very carefully. And perhaps patients should not assume that medications like NSAIDS that they can buy over the counter are completely safe.
Share your own experience with atrial fibrillation in the comment section below.


Chris
I had my 5th episode of Afib in December 2023 which was triggered (I believe) by doxycycline that I began taking for Lyme disease. I had to wait until I was finished with the 30-day course of doxycycline to have cardioversion (4th time for me in 30 years). I then underwent a cryoablation procedure in April 2024. I have had one brief episode of Afib since. I am using a CPAP machine nightly (another cause of Afib) and do not drink alcohol.
MJ
It took several years for my internist to agree that I had a problem. I finally started recording my BP & irregular heartbeat in a journal. He finally agreed that I needed to wear a monitor. I had a bad episode while I was wearing the monitor & the company watching the monitor called & told me to go to the hospital. My internist still did not recommend a specialist, but the monitor company & got me set up.
Keith
A family member had recurring episodes of a fib/a flutter that were about to lead to potentially dangerous drugs to suppress the dysrhythmia. After she completely discontinued her alcohol intake (1 vodka martini and 2 glasses of wine each night) her fib/flutter has not returned. Are you aware of any data to support this correlation?
Julie
How about thyroid out of normal range, too high or low? I understand that can trigger heart rhythm issues.
Marty
I had an episode of SVT right after a dose of my shingles medication. Sent me to the ER
Jeanni
Six years ago I was diagnosed with AFIB and put on a calcium blocker which helped. Then four years ago I started drinking two 6 oz. glasses of concord grape juice daily which makes your blood less sticky. What the doctors call a blood thinner really makes your blood less sticky it does not thin your blood. Since drinking the grape juice I am now off the calcium blocker and have had no AFIB episodes. A plus for me is that a varicous vein in my left calf that I have had for over ten years is pretty much gone.
Aleksu
Several tick-borne diseases I have are the cause of my a-fib, but none of my cardiologists know anything about Lyme Disease or Babesia. One especially dreadful cardiologist flat out stated: “Your Lyme Disease did not cause your A-Fib.” There are tons of papers on the topic. There is also a connection between a-fib and clotting disorders caused by mRNA vaccines. I am not anti-vax, but I am anti-a-fib! I hope some researcher looks for a way to adapt the technology to allow a-fib patients to safely take the Covid vaccine. I haven’t continued with the vaccine boosters because of its potential clotting effect, at the suggestion of a doctor.
Katharine
I found that quinine is a trigger for me–in my case gin and tonics. I now have a pacemaker (for other reasons) and have not had a negative report in two years.
Jessica
Gee, do you suppose there could be a correlation between the current alarming increase in the rate of A-fib and the recent recommendation that any blood pressure reading of 120/80 requires extremely aggressive treatment with the very BP meds that are listed as A-fib culprits in this article? Is this another example of “medical dogma” winning out over data and common sense?
Modern medicine is profit driven, not patient driven! It seems to be doing a great job in creating more problems, requiring more visits to more specialists, who are prescribing more and more meds, which cause even more problems, requiring ever more meds, visits, procedures….well, you get the picture! It’s time to get off the modern, profit driven, medical merry-go-round; don’t you think?
CJ
My mom was on two blood pressure meds while suffering occasional Afib episodes. We later learned that she had hyper-obstructive cardiomyopathy, and her low blood pressure was triggering the Afib. Her heart simply couldn’t pump blood effectively past the obstruction with the low pressure (110-115 systolic) Once we set her target BP at 130-140 systolic, her afib episodes decreased significantly.
Carey
Albuterol for asthma did it for my mom. Turned out that was COPD. Her best friend, who was 15 years older and also had COPD but not afib, outlived her by several years. It was the afib that caused her to die so young.
Sharon
Was put on Norvasc and within a matter of weeks now have AFIB. Doctor just ignoring me. Be careful, and get a 2nd opinion. Sometimes the doctor may not really be helping. Hope nobody ever has to go thru this nightmare.
Brad
3 days after taking Benicar(Olmesartan 40MG) I went into AFIB. Stayed in AFIB for a month. Took 2 cardioversions to set it back straight. Beware.
AF is a pain
USA
MSG.
If I cook my own food I don’t get AF. But if I go out to restaurants there’s a fairly good chance I will get an attack. I was surprised this article didn’t mention a link to the increase in use of MSG, and its many pseudonyms in processed foods to the increase of AF.
Mitchel
Brooklyn, NY
Thank you for all the very interesting comments. Does anyone here know about Ventricle tachycardia? My defibrillator went off for the first time 2 weeks ago, and recorded a number of incidents that had resolved without the defib going off, but it’s very dangerous. So the doctors want me on amiodarone, and I’m looking for natural substances, maybe bergerine? I already take around 550 mg of magnesium (aspartate and citrate) every day, plus many other nutrients. Thanks.
Jane
Indiana
Anyone having Afib problems should have their thyroid checked with what they call a FULL PANEL not just the normal thyroid test. Plus, it should be read by someone who knows what they are doing. Too many people are going misdiagnosed. If a person is very overweight, they could have a hypothyroid. If the full panel thyroid test shows the thyroid to be even slightly off, it should be treated with a NATURAL thyroid not synthetic Synthroid. Also, I agree about the importance of supplementing with magnesium. I
John
Alamogordo, NM
Every time I get albuterol, I end up with AF. I have a cardiogram, and it shows no A; twice yearly EKG at the Dr. office shows no AF. I am on rat killer AKA coumadin, and it is causing denial of treatment for various problems. I have been denied treatment for back problems, toe infections, and other problems. They require “clearance” for coumadin, and my cardio guy won’t budge.
Today I meet with the Dr. and take myself off blood thinners and pacer 1, because the only time I show AF on paper is after albuterol treatments. I figure from what I have read here, I will feel better. I am not afraid of ablations as I have had two in the past for tri and bi Gemini (avandia). But I think they have to see it to treat it, and I have not seen AF except a few times in the past.
Jim
Va
I just attempted a half marathon; I had several recurring bouts with tachycardia. This was while running, and also after I was walking back to the finish line. What happened? I’d taken Aleve the night before (ibuprofen gives me a rash.) I did it for some carpal pain that I hadn’t been able to resolve manually (until I changed techniques and it seems to be working.) Considering the following, it appears that the only causative agent was an NSAID.
I had done two swim races the week before, a 1 Miler and a 5 K ocean swim. No issues, even though I worked my butt off and won my age groups. The week before, I had run 13 miles in a training run, along with 10 pushups every half mile, losing 7 lbs in the process (not smart, but…?) No issue; not one.
Several years ago, I did a trail half marathon. I remember – now – taking Aleve prior to the race. During the race, I had an episode where my heart jacked up to 210. It eventually came down, and I finished the race with my normal 150-160 HR.
Also remember doing a 10 mile swim and taking Aleve. Well, 10 miles is like 30-40 running. I did it preemptively, and foolishly. I had a few flutters then, but thought nothing of it.
Now, it all adds up. As a friend of mine texted me last night: “Aleve it alone!”
Charles
TN
Have had A-Fib for 15 years and found dehydration & stress are definite contributors. NEVER let them use paddles unless life-&-death matter. Took 6-months to get over young kids’ experiment, twice with no help. My whole personality changed after the paddles until I had another A-fib and came back the usual way. I had told him to give me something to bring down my BP and something to lower my heart rate & he gave BP meds but then chose to Paddle before giving anything for high heart rate. I treat my own now with Benicar for BP and Lorazepam for relaxation – then couple baby aspirins for potential clots; then lay back and relax and usually kicks back in within 1-2 hours. Saves about $5000 ER bill.
Storm
Arizona
In 2016, I ended up in ER a few days after taking Fluconazole. Recognizing that the problem was caused by Fluconazole, I resisted a lifetime regime of blood thinners. I was a victim for a while, however. After several months and every test known to diagnose heart disease, I finally got over the problem. Here’s the rub; I ended up in ER again with Bell’s Palsy, a simple diagnosis with no explanations or attempts to find the root cause. The ER doctor prescribed Prednisone and an antiviral. I researched Bell’s Palsy and discovered that Mayo Clinic’s online site indicated that Prednisone and an antiviral medication, the usual meds for Bell’s Palsy, are ineffective.
Well, I neglected to check A-Fib/corticosteroids and decided to take the Prednisone and antiviral (Acyclovir 200) because of a lingering sinus infection. After two doses, my heart started the A-Flutter. BEWARE OF CORTICOSTEROIDS. I am learning. My research shows that many, many drugs are responsible for getting the heart out of rhythm, including over-the-counter NSAIDS. I am 85 and don’t take any prescriptions regularly. I am not a helpless 85 year old. Big Pharma doesn’t care if they kill us (follow the money), and doctors are mere puppets to the system. America’s best hope for healthcare would be to drain the Big Pharma swamp.
I am trying to convince my doctor that the Bell’s Palsy that I have had for two weeks is caused from Mastoiditis connected to the sinus infection. A CT scan was necessary to rule out stroke but didn’t show anything else! I question the reliability of the doctor reading the CT scan. The CT scan should be re-analyzed. Tell that to a doctor. You can’t do that; you might find that something was missed! I am learning to mistrust the entire medical system.
Check out electromagnetic fields and A-Fib. Electomagnetic fields can affect the heart. I have gotten rid of my wireless electronics as much as possible. I am not taking any chances. I don’t want a lifetime of blood thinners, blood draws, etc.
JIDude
USA
Just saw this thread a couple years late, but I think my experience is worth documenting somewhere.
Was taking generic escitalopram (name-brand is called Lexapro) for anxiety and started getting these. Cardiologist said benign PVCs, they just happen. Well, I was getting it a dozen times per day and it was very uncomfortable. So I tried eliminating medications one by one for several days each.
First to go was levothyroxine for thyroid. Nope, condition persisted. So got back on that med.
Knocked out lisinopril for BP. No luck, got back on it. Dropped fenofribrate for high triglycerides. Still had PVCs, so went back on the feno.
At that point, the only other med was escitalopram and I couldn’t imagine it was doing this to me, so I didn’t both with it. Well, I got a prescription refill of the escitalopram and noticed that the maker of the generic drug had changed. Bam! Immediately, lots and lots of PVCs. So I quit the escitalopram for a week and the PVCs went away. Took another one and they came back. Got off it and they went away for good. Doc prescribed a week’s worth of name-brand Lexapro and I took one and had only a couple of PVCs, but didn’t want to fool with it anymore. I am sure of two things:
– Escitalopram may trigger PVCs in me.
– The generic version triggered literally hundreds of PVCs per day!!
My belief is that the generic makers have poor quality control, or are deliberately putting inferior “carrier” substances into their tablets to save money. If the heart palpitations ever come back from taking another med, I’ll ask the doctor to get me name-brand, made in the US or Europe, not some back alley in Bangalore, and see if that solves the problem.
Mike
MA
I’ve had 2 a-fib trips to the hospital in the last month since I’ve been put on a diuretic. I’m convinced there us a correlation.
Jacy
TX
The diuretics cause loss of magnesium and potassium. If the level of them becomes too low, you can definitely get heart palpitations/A-fib symptoms. You may need to take supplements while on the diuretic.
John
Florida
I’ve had about six occasions where my pulse accelerated rapidly after an evening of a couple of bourbon Manhattans and a rich chocolate desserts. All subsided 1-2 hours later. The last episode was with three light beers and heavy sugar desserts.
Slowly coming to think the excessive sugar is more detrimental than alcohol.
Haven’t seen any places where the triggers of afib are evaluated.
Karen
Canada
Magnesium, for muscles! Your heart is the biggest one. Proper rest and nutrition are our problems. Our foods are devoid of it, and it makes us sick. If you take probiotics and eat whole foods, with nutritional supplementation, eliminating ALL grains and sugars, as well as any and all GMO foods, you will see your health return. It’s the food that is making/keeping us sick. That’s why it’s a global problem.
Jerry
New jersey
I am a 76 year old male. I never had an afib problem until one week after surgery (3 years ago) where I had an aortic heart valve replaced. I am convinced that there is a correlation between my afib and this surgery.
Nan
TX
I developed A-fib as a reaction to spinal cortisone injections for back pain. Eventually the A-fib stopped and has not returned. I have had no more cortisone injections, and do not plan to again!
Cindy M. B
Seattle, WA
I’ve written this before, but it’s worth saying again:
I was (to my horror) dx’ed with Afib 5-6 years ago now. What the dr’s tell you IMMEDIATELY is that alcohol intake is the biggest risk factor in developing Afib… and yes, I’d gotten into the habit of drinking about 3 drinks a day, though spread waaay out. They said NSAIDS were another big risk factor, and yes I’d taken Advil and Aleve routinely for sports pains. After a year I had an ablation, which immediately cleared up the Afib. It’s quick, simple and certainly nothing to be feared.
But the stupid MEDS! The standard meds for Afib are (1) an anticoagulant and (2) a beta blocker. Those horrible meds really slowed me down, made me feel like 80. This was very apparent when skiing and backpacking. ALSO, the meds gave me nasty, nasty dry eyes every single morning (which went away immediately when I stopped the meds).
If you are continuing on meds because you fear an ablation, for heaven’s sake get the ablation! Mine stopped the Afib immediately and I’ve never looked back (though I HAVE cleaned up my act a bit for good measure). Cheers from Cindy in Seattle
Mary
I started with hyperthyroid problems in the 90’s. At the time my heart would be racing but I wasn’t told it was my thyroid causing this. My doctor had me go to a cardiologist and he said I had A-FIB. I didn’t think it was that serious at the time, and over the years he would suggest I have my heart checked with the whole works.
I really never noticed my heart skip over the years, but I did have attacks if I had MSG. With in an hour I would have the shortness of breath, palpitations, and other symptoms. A year ago I thought I was having a heart attack and went to the emergency room at the hospital. I went to the cardiologist and he put me on Eliquis. Over the years I used all the above medicines for arthritis plus others not mentioned. I really don’t know what to blame it on, but do have my suspension it was the thyroid that started it all.
Raed
Iraq
Many years ago, I suffer from AF. from time to time became a guest in the hospital…
At first, i took (Digoxin) for a long time, then (Cordarone),
And at last, I’m keeping on (Inderal) as a daily treat.
At the hospital, they add (warfarin and Meto) as injecting.
(so I feel I’m a field of treatments)
Small note: I have a cyst on my kidney.
Another note: I’m smoked.
Many thanks and my best regards to you
Raed, Iraq
age 56y/o
Jack
Wisconsin
My AFib has disappeared since I added 200 mg of magnesium chloride in a liquid suspension, split between morning and bedtime. Premature atrial contractions also now very rare as well. None of my medical caregivers ever suggested trying magnesium. Magnesium chloride in suspension is well-absorbed, with no laxative effect–important to me because I have villainous colitis.
Karen
That is what I believe also. It’s all in the food
Bill B.
Fort Worth Texas
About seven years ago at age 68, I was suffering with tachycardia. This was very frustrating for me because I NEVER smoke, drink alcohol, or do drugs. I also exercise, have been normal weight, and do not have diabetes. Nothing seemed to control it and no one could explain it. I finally had an A-flutter ablation procedures. It worked! I was normal for six years. Fast forward, six years later, I started having tachycardia again at near 75 years old. Unfortunately, I soon had a stroke. I remembered the importance of getting treatment fast, so I did and was administered a clot-busting drug in time to not have any damage. I just completed my second ablation procedure, this one for A-fib. I will be able to better judge my long-term condition after getting off some of the drugs they have me on now. In summary: Sometimes genetic predispositions and aging combine to cause these heart irregularities. There is no one solution since all of us are individual, highly complex, electro-chemical systems. Take your condition seriously, study, and combine the best of naturopathy with modern technology. And keep reading the Peoples Pharmacy!
Jay
Houston
Inspite of surviving a stroke in my forties, and two heart attacks in my fifties, I was lucky to recover enough to play tennis with seniors of my age into my eighties ( I believe thanks to full dose of 325 mg aspirin daily started by my cardiologist).
Early this year when my HMO shifted me from Humalog to Novolog I started getting out of breath even during warmup for tennis. When I complained to the my doctors about change of insulin, they did not believe my opinion on the change of isulin. Even minor task of picking up newspaper from the front lawn ended up being out of breath.
I finally ended up in ER where they diagnosed it as early stage of CHF with my weight going up nearly thirty pounds. Hospital staff put me on water pills to bring down my weight and swelling of my legs.
I am now back on Humalog and hopefully can recover enough to hit a few balls with my tennis buddies.
Brenda C
Indianapolis
I am 66 and I believe HCTZ was my initial trigger of aFib AND incontinence 5 years ago. the 2 problems started a few months apart. Today if I OD on sugar it can trigger aFib. I can take 1000mg Chromium and it will disappear in 30 minutes. not much of a salt eater, but once I ate a bunch of potato chips and it triggered aFib. chromium won’t work on salt so I had to wait 3 hours for it to pass.
Susan
I was recently put on HBP medication and have notice so many odd side effects, one being my heart rate. I would get a rapid heart rate and lightheadedness at night. I also workout and eat a low carb high fat diet. I read all your articles and have connected so many dots!! I drink Gatorade or Pedialite everyday plus take potassium and magnesium. My goal is to reduce my weight thus lower BP and get off meds. Pretty sure I won’t need meds by my next doc visit. I can’t thank you enough for your enlightening articles. Medications in general are risking. Overall good health and diet is quite easy to achieve.
Carole
Ohio
In my case Thyroid medication caused my AFib. When I stopped taking Levothyroxine for Thyroid, the atrial fibrillation ended. Also, experienced a brief episode of atrial fib after taking Omeprazole for 1 1/2 months for stomach ulcer. Had to stop that medication as well. Physicians do not check drug list for possible cause of AFib !!
Anna
Bangor
I started out with paroxysmal AF at 63, out of the blue. Ten years on, it has developed into a permanent condition which has impacted greatly on my lifestyle. The only option now is to control the heart rate as drugs are no longer effective in controlling the arrhythmia.
I take a cocktail of different drugs, with no professionals knowing the effects of this polypharmacy. My quality of life is greatly diminished and I am at high risk of a stroke. The only drug I took before developing AF was omeprazole. Whether this was a causitive agent, I just don’t know
Barbara
Arizona
About eleven years ago, I was diagnosed with Barrett’s Esophagus and was prescribed Nexium, 40 mg. I developed diarrhea and Atril Fibrillation within three weeks. I tolerated the Nexium 40 mg until the past year when I made my first appointment with an NMD and told her I would like to stop Nexium for the severe heartburn that I was having all the time if I didn’t take the Nexium. She advised me which foods and liquids I should stop, which I did. However, I decided to have a test on my esophagus that showed that I had developed a Hiatus Hernia which allows stomach acid to flow backwards up the esophagus. Hence, the NMD said I would not be able to completely stop taking Nexium, but was advised to try 20Mg of the generic for Prilosec. I find that 20Mg of that ProtonPump tablet and the elimination of several foods and liquids has helped along with five different natural substances the NMD recommended I keep on hand. Coffee was first to go on “my list.”
Cecilia
california
My husband was given amlodopine ‘to try’. Within 3 weeks he developed shortness of breath and could barely walk across the room. I researched all the medication he was taking and one had a listing for Afib being reported. So we went back to his doctor who did an EKG and diagnosed Afib. Instead of looking at why all of a sudden this occurred, the MD immediately wrote out prescriptions for warfarin and digoxin. After arguing about this and telling him what we had read we left the office. We didn’t fill the prescriptions, discontinued amlodopine on our own and within 2 days, my husband felt and saw an immediate change.
We went to the MD on the 3rd day and the EKG was normal. After we told him what we did, the MD dismissed the connection between amlodopine and the Afib episode. It’s been almost 2 years with several follow up visits with the cardiologist and all EKGs are normal, no repeat episodes but he too won’t connect the dots to a drug induced Afib episode.I hope this anecdotal experience will help someone to do their own investigation and research and NOT be afraid or timid to question the medical community.
DICK
ILLINOIS
I just turned 80 and just received a diagnosis of afib. I have been taking trazodone for about 5 years to help with getting to sleep. After the diagnosis and reading that trazodone can be a trigger for afib I quit taking it and will just deal with the sleep problems. The occasional (3 or 4 a day) afib events that would last for a minute or up to five minutes pretty much stopped within a couple of days. I wore a monitor for 30 days and would have a short event maybe every other day. I went thru a battery of physical and blood tests with no change in the diagnosis. I have also started taking a magnesium supplement and eating a banana each day for the potassium. I have a prescription filled for eliquis but am fearful of starting it after researching the potential side effects and am hopeful that the potential for clots is low due to the short duration of the afib events and the time between events. Am I taking too big a stroke risk?
Daiv
Washington
I am almost 67 having had Atrial Fib issues for 20 years or so. I exercise fairly heavily which brings on an episode very early the following morning. My prescribed regimen includes 150mg of Propafenone and 20 mg of Propanolol (beta blocker) 2x daily. I take Standard Process supplements (Cardio and B vitamins). Last summer I was urged by 2 friends to increase my electrolyte and mineral intakes. Bingo! My episodes were severe (12 hour) and predictable but now infrequent and mild (4 hour recovery). One of my chiropractors have moved to Seattle and picked up as personal assistant to Michael Phelps. He recommends a product called NUUN for electrolyte (better than Gatorade which is loaded with sugar) balance. I can say that I have not had an episode of A-Fib after a dissolved NUUN tablet in 500mg of water nor after drinking Gatorade. I was about to go under for an ablation procedure. Instead I went on a grueling 5 day backpack trip last summer with no episodes. Can’t hurt to give a try!
Esther
British Columbia
I am a healthy white 68-year-old female. I have never taken ongoing medication. I have normal blood pressure. I have also been diagnosed with atrial fib. In my research, I discovered that people have recovered from this by increasing their intake of Iodine.
Here is the article I read that I found encouraging.
http://www.healthsalon.org/435/iodine-and-cardiac-conditions-afib-arrhythmias/
Thanks for your site and your information.
Taz
Wisconsin
I’ve had AFib for a year now. It came on suddenly after taking only a couple capsules (a smaller dose than recommended) of an ashwagandha KSM-66 supplement.
Linda
South Carolina
When a woman goes to the Emergency Trauma Unit, (MUSC, etc.), with symptoms prior to having AFib and a heart attack, the medical professionals should be able to identify the situation and not call it indigestion. They knew that I had been taking a diuretic, but did not suspect that I had lost nutrients. That fact was identified four days later, when I had an AFib episode which resulted in a cardiac arrest and death. Thank the Lord, I was revived.
I have to stay on top of the medication(s) that I am asked to take, asking question- why, what, what is the history of the meds and for how long should I take them, etc. I have a great primary care physician now, but realize that even he has to receive info about my body from me. This info is not always presented in medical journals. I wonder why I should take diltiazem when I only had that one (near fatal) incident caused by potassium depletion? Why has diltiazem caused me to urinate more often than even the diuretic that I used to take? I am still looking for answers. Thanks.
Karen
North Carolina
I began to have a very irregular pulse using Celebrex 100 mg once per day. I know that was the cause, because I would skip a day or two and I would have no symptoms. Then when I took another dose the arrhythmia would return. I looked this up on the Web and the only place I could find this in a study of fruit flies! Well, maybe that’s in my DNA! :)
Rick
The facts are that the risk of taking any of these medications outweigh the benefit you will receive from then. Pharmaceutical companies have planned this. Let’s call it premature obsolescence, mortality, coupled with more medications to deal with the morbidity.
nathan
Dallas
Hi, one of my wife’s friend had a lump in her breast. They removed it and she was on chemotherapy and radiation for a period of time. She finished all the regiments but after a short time she noticed having short breathe and she can not do her regular physical activities.
Now, she has been diagnosed as having congestive heart failure. Is this known that chemotherapy can have such a devastating side effect?
Sincerely
Nathan
Trish
Illinois
This article is such a revelation! Over the years, various things have caused me temporary irregular heartbeat. Aspirin did this, as well as allergy medications and all of the statin drugs. I was hospitalized and given prednisone in IV form for a bleeding disorder, after which I had to stay on prednisone in pill form for 3 months. Because of this, I now have permanent atrial fib. I have told many doctors that aspirin and other drugs cause me heart problems, but they didn’t take my concerns seriously. So now I face life with this scary heart problem, taking even scarier drugs for this condition. I have all of the symptoms you mention in the article. It is hard to get through most days. The cost of the drugs I now take is prohibitive. I’m trying not to be angry about this, but it has changed my life in an extremely negative way. Thank you for publishing this eye opening article.
Carol
Texas
Consider all the young people in affluent countries who drink Red Bull and Monster drinks and other high caffeinated drinks for many years. Seems like a cause for A fib.
Judy
I used to have afib. It took years for me to figure it out; it was from smoking & drinking coffee at the same time. It must have sent my blood pressure skyrocketing; I went to many Drs. – no one asked me about the smoking or coffee (also Pepsi) and I finally figured it out myself. I have a very sensitive constitution.
Joan
SLC, Ut
I have had two episodes of AFib, both ending in the ER. After the last one, I started using Magnesium glysinate every night before going to bed. It’s been at least two years, and I haven’t had any more episodes.
Larry M
The proposed causes of hypertension, diabetes, aging, and medications do not seem to fit my situation. At the age of 62 I developed paroxysmal atrial fibrillation. I was, and still am, normal weight (5’9″, 165 lbs.), moderate BP (120/60 or lower), no diabetes, age 62, and the only medication I was taking was occasional Tadalafil.
The conditions cited above are associated with aging, as is atrial fibrillation. However, don’t forget that CORRELATION DOES NOT IMPLY CAUSATION.
By the way, at the age of 67 a circumferential pulmonary vein ablation (CPVA) was performed and was the best decision I’ve ever made. I awoke on the table in the recovery room feeling better than I’d felt in two years, and it’s only gotten better since then. I’m 72 and hike in the mountains, cycle, and snorkel with the young folks.
Kathryn
Scottsdale, AZ
I am about to turn 70, and I have experienced arrhythmias since I was in my twenties. I’m very careful about what medications and supplements I take. Have had very many EKGs over the years and especially recently, and arrhythmias are never, .ever detected. But at home and when I am out, I often experience the fluttering, pounding, tachycardia, shortness of breath, and occasional chest pain. Have had the full gamut of heart tests and nothing is ever found. So I feel my only chance of preventing a stroke is prayer. I do appreciate articles like this that remind me what NOT to do. Thank you.
Brenda Clark
I have a very mild Afib. It stops on it’s own. I take 25 mg Toprol XL, 20 mg Quinipril, and 325 mg Aspirin. I also take Armour Thyroid and have been told this might be a link. But I took the thyroid med over 10 years before any Afib incident. I had symptoms 2 years before it was diagnosed. I have kept a journal. I have discovered SUGAR is a trigger for my Afib. It can be too much sugar, weird types of sugar, and alcohol. also salt. If the trigger is any type of sugar, I can take a 1000mg Chromium tablet and it stops in 30 minutes. one time it was salt and I had to wait it out … 3 hours. One time I forgot to take my meds and it felt like Afib was coming. So I need to remember to take my meds as instructed.
Interesting though, my blood pressure med used to be part diuretic and an MD changed it to plain quinipril. Also, an MD put me on Nabumetone 500mg 2X daily. then another MD took me off it. These happened about the time my Afib started.
Jan
midwest
I am 58 year old female and not on any medications. I have had palpitations for the last two years. I especially notice it when I sleep on my side. I have not gone to a heart specialist yet. Are there any natural remedies for this? I have no side effects from this either other than being aware of the pounding, erratic heartbeat every few minutes or longer. Even the timing of it can vary. I do notice if I have stressful times, caffeine, or a glass of wine, it increases. I’m not sure if being on medication will be beneficial especially seeing all the side effects. Any information you have would be appreciated. Thank you.
MR
I used to occasionally feel heart palpitations at night soon after going to bed. They didn’t last long. I have not noticed them much at all, though, since I’ve increased my magnesium intake by adding 800 mg of an amino acid chelated form to my usual magnesium malate tablet.
I also take nattokinase sometimes, as it seems to be excellent at dissolving clots in the blood.
Anna
Florida
I had about a half dozen trips to the emergency room before I came across Dr. Mercola’s suggestion to take Ubiquinol, a form of CoQ10. I now take 100 mg. both morning and night and it has been 6 months since I had atrial fibrillation. I buy it at Costco or another big box store and the price is around $30. I was so disgusted with what blood thinner and the threat of ablation did to an otherwise healthy person, that I took my own treatment in hand and I haven’t had cause to regret it.
Molly
Santa Fe, NM
I have the common form of occasional arrhythmia. I am 72 but don’t take any medications at all. The arrhythmia correlates perfectly with caffeine and/or alcohol consumption, particularly with caffeine, and sometimes with general stress and anxiety. Years ago, when I was first entering perimenopause, I had my first heart flutters and went straight to the doctor, where an EKG confirmed the phenomenon but nothing was said about the cause. As I was leaving the office a nurse leaned over and suggested softly that I might try switching to decaf coffee. I did so and gradually quit drinking any coffee at all, and the flutters didn’t come back for a few years (until I developed a chocolate habit). Eventually cardiologists figured out that 1 in 10 women are sensitive to caffeine. The other factor that I’m very curious about, however, is the EMF from both electrical wires and wifi, which now permeates our world, even more than the various medications you’ve listed. Will we find out 20 years from now that this too correlates with arrhythmia, insomnia, and….what else?
Jim
Michigan
I started having atrial fibrillation when I was about 40. I will be 69 in May. I have an event infrequently. Sometimes once a year and sometimes as infrequently as every five years. As I have gotten older they have occurred with less frequency. Obviously there are a number of factors that that cause atrial problems. Mine seems to be idiopathic. I believe that on some level stress can be a significant contributor to creating chemical imbalances that contribute to atrial problems of this nature. I am not medicated other than a low dose blood pressure medication and a baby aspirin. I make every effort to keep well. I walk 3 miles a day, meditate daily, I take a magnesium supplement along with a multiple vitamin and I keep hydrated. As least for now this seems to work best for me.
Carey
Chicago
My mother was convinced that her asthma medication, Albuterol, was the cause of her AFib. She only took it once, but the AFib didn’t go away.
Deno
What kind of doctor says “I would really strongly advise that older people be very careful with using these drugs. They don’t do anything except relieve pain. Pain is a nuisance, but dying is a nuisance, too.”
If all a drug does is relieve pain, I want that drug.
Brenda
Texas
It was determined that naproxen caused the atrial fib that I experienced a few years ago.
No naproxen — no atrial fib since. The doctors could not determine the cause, but I
figured out finally that every time I took naproxen, I had an episode.
Noah
Chapel Hill, NC
I took NSAIDs including Naproxen on a daily basis and in heavy doses for in excess of thirty years. After a stroke that the onboard aspirin probably ameliorated I was put on Clopodigrel and stopped all NSAIDs due to interactions. In a year or so I developed afib and am now also on Eliquis. Ouch! Is it possible that getting off NSAIDs (suddenly) can also trigger afib?